Unity Provides Managed Technology Services and Member Call Operations for Health Insurance
Unity’s mission and offerings increase the profitability and efficiency of our clients' operations while providing preeminent support to plan employees and members. Unity believes our brand of being a high-performing lifeline to end users in their use of technology is just the beginning. We recognize we must deliver on cost reductions, innovation, security, creative customer experience (CX) and client satisfaction every day.
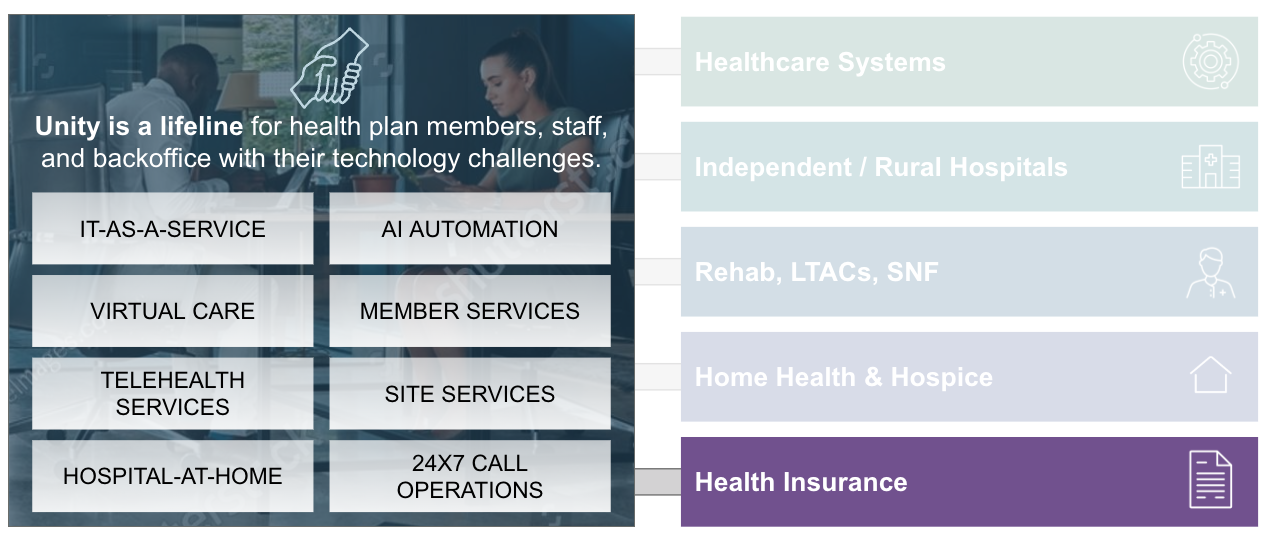
At UnityBPO we support:
- Plan members in understanding their health insurance
- Insurers’ staff in their use of technology
- Backoffice in efficiently using tech for RevCycle, Claims Processing, HR, etc.
Through our robust portfolio of products and services, Unity brings the skills, experience, tools, knowledge, and best practices to make human-technology interactions simpler, easier, faster. This portfolio reduces costs, increases productivity, and meets requirements for regulatory compliance.
Insurance Operational Optimization: Reimagining End-User Services. Delivering Value.
Member Services
Call center for claims questions, eligibility, demographic changes, provider changes / searches, benefits explanation, assistance with Appeals & Grievances (A&G), basic inquiries.
Reduce costs and improve Return on Investment (ROI). Implement a concierge member experience. Enhance security, compliance, and quality.
AI / Automation
Generative AI Assistants for end-user support / services, Co-Pilot intelligent agents, Large Learning Model (LLM) / knowledge development and facilitation.
Reduce costs and improve ROI. Enrich member experience. Enhance security, compliance, and quality.
Robotic Process Automation (RPA)
RPA to automate claims registration and processing, regulatory compliance, policy administration, and form registration.
Lower processing costs. Gain operational efficiency. Reduce error rate and delivery risk.
IT-as-a-Service
Robust IT-as-a-Service offering for health and specialty insurers.
Includes CTO/CISO, compliance, mobility, claims / care management system support, EHRs, infrastructure, managed print, security, automation, high-touch support, asset management, and on-site services.
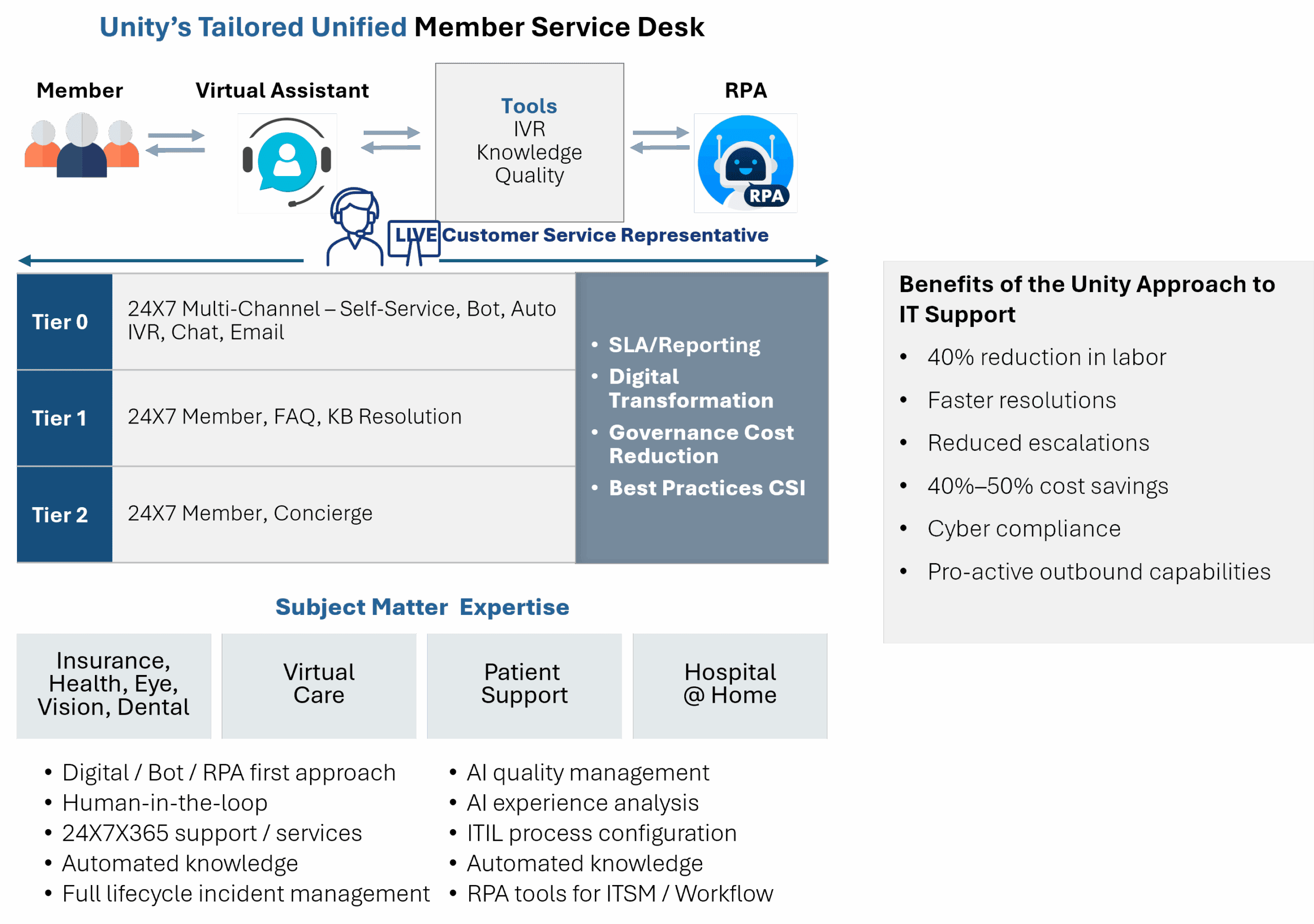
Technical Service Desk
As an IT Managed Service Provider (MSP), Unity provides both member service call operations and IT support for insurer’s employees, including Tier 1 and 2 service desk. Beginning with our Digital Front Door, we use an AI First approach to remote service desk
Lower costs with automation tools and platforms. Provide a better support experience for employees and members.
Unity Co-Sourcing
Unity’s Co-Sourcing Model allows clients to blend their top talent with proven, high-performing staff while you maintain control.
Gain a team who is a cultural fit, scalable, and highly experienced at less expense than insourced resources, all while keeping your top talent.
Staffing/Projects
Upgrades, technology implementations, refreshes, real estate, Mergers & Acquisitions (M&A), project management, CTO, architecture, staffing, temps.
Realize lower costs. Increase customer service representative (CSR) utilization with proven expertise at competitive rates.
Reimagined End-User Services
Remote Services
Tier 1 Service Desk
- Technical Support
- Clinical Support
- Member Support
Remote Support Team (T2)
- Major Incident Support
- Advanced CRM Support
- Advanced Technical Support
On-Site Services
On-Site Support
- On-Site Face of IT
- Executive Concierge
- Incidents / Break-Fix
- Service Requests
- Projects
- Managed Print Services
Continuously Shift Work to Low Cost • Identify and Implement Automations
A Model That Makes Sense
- Daily connection and communication with all areas
- Daily on-site support for critical systems
- Tele-health / virtual health
- Multi-tier support / business-vendor relationship management
- Executive / VIP 24X7 + support for home and office
- Intentional Shift-Left process reducing costs
Extraordinary Value
- Reduce escalations
- Proactive resolution means issues found before reported
- Engender extraordinarily high customer satisfaction
- Experience zero backlog for IT incidents / services requests / refresh
- Incumbent capture means you don’t lose talent or knowledge
- Transform traditional field services to deliver excellence
Unity’s Member Services Employ a Concierge Model
Designed to Provide a Personalized, High-Quality Customer Experience
Unity Value:
Unity’s solution to member support is both low risk and low cost. Our clients experience:
- A co-sourcing model that results in lower costs, improved performance, and better platform costs
- An AI First call operation, which can lower your insourced headcount / costs
- Stable rates through Unity’s use of incentive-based pay to control rate creep
Reimagined AI-Centric Healthcare Insurance Member Service Desk
Unity ITaaS Approach and Value
Unity’s comprehensive, fully managed IT services include managing cloud, infrastructure, security, on-site services, analytics, managed print, network, communications, projects, and strategic IT planning. By outsourcing routine IT tasks, your internal teams are freed up to focus on delivering healthcare to patients. You gain operational efficiency and innovation.

Unity Value:
- Fractionalized labor, where you are paying for what you use
- Fractionalized tools, platforms, and licensing, where you are paying significantly less
- AI strategy and implementation further lowering costs
- Predictable costs, much less than insourced IT
- Proactive approach
- Access to HIT community expertise and greatest hits
- GPO-like deals and financial benefits
- Scalability
- Best practices and proven processes
- Reduced downtime
- CIO / CTO / CISO expertise
- We hire incumbents, who gain training, expertise, and opportunity for advancement
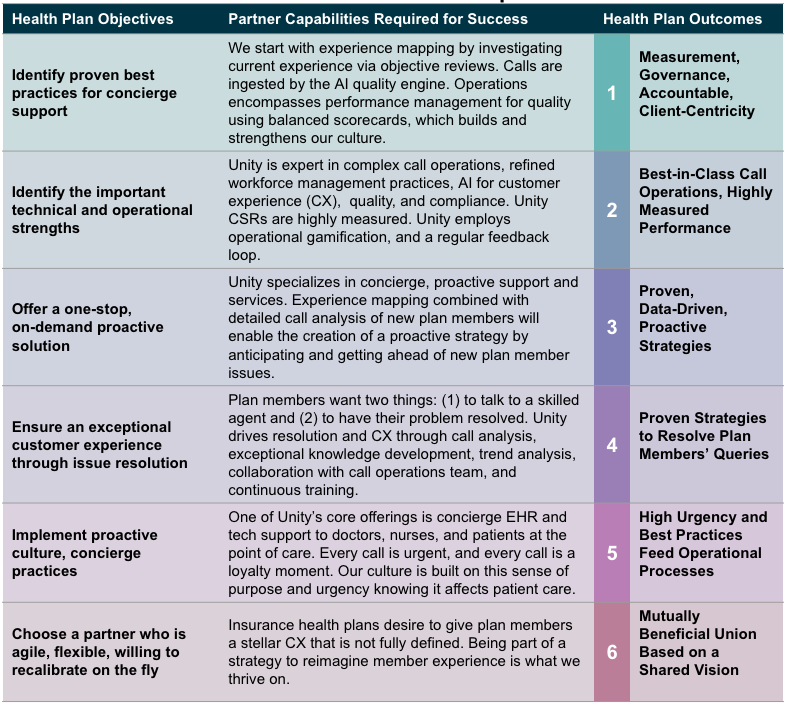
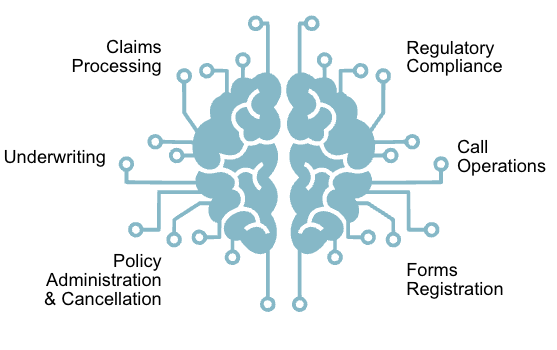
Automation in Health Insurance
AI offers significant benefits to the health insurance industry to include error reduction and compelling cost savings, as well as productivity gains. By carefully considering these benefits and challenges, health insurance companies can leverage AI to create an efficient, accurate, and customer-centric insurance landscape:
- Claims Processing – Claims analysis, automated verification, error recognition, pattern identification
- Fraud Detection – Suspicious pattern identification, predicative analytics, false positive reduction
- Underwriting – Risk prediction with higher accuracy, future health issue prediction
- Customer Support – Chatbots and virtual assistants provide 24x7 support answering policy-related queries and assisting with claims submissions—a more personalized CX will promote loyalty
- Operational Efficiencies – Automating data entry, claims filing, policy renewals
Automation Opportunities
Automation Value
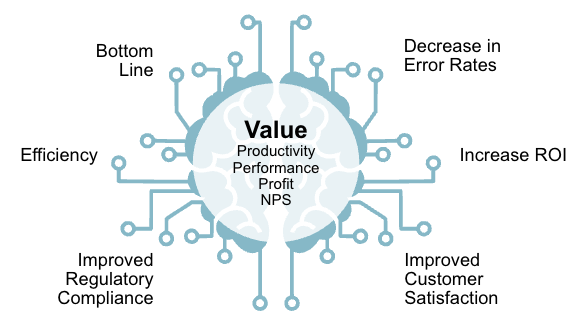
Unity Brings and Implements Integrated AI Solutions Supporting Members and Insurers’ Staff
AGENT ASSIST
AI Agent Assist
Interaction Notes / Summarization
KNOWLEDGE
Knowledge Development and Facilitation
Security / HIPAA Compliance

LINGUISTIC CAPABILITIES
Customer Sentiment
Multi-Lingual Real-Time Interpretation and Translation
AI BOTS
Gen AI Chatbots and Voicebots
Customer Personalization
What Are the Benefits of Using Unity’s AI Platforms?
Agent
Assist
Always On
24x7x365
Availability
Better
Customer
Experience
Rapid
Response
Accurate
Triage /
Knowledge
Improved
Analytics
Higher Productivity
Omnichannel
Access
Lower Operational Cost
Seasonal Scalability
Personalized Interactions
Better Compliance

Unity’s Operational AI
Unity’s integrated AI platform for end-user services leverages artificial intelligence to streamline operations, enhance agent / technician performance, and improve the overall customer experience. These platforms integrate with existing contact center technology stacks and offer features like AI-powered chatbots, real-time agent assistance, predictive analytics, and conversational intelligence.
By automating tasks, providing insights, and offering personalized support, AI-powered service desks with skilled remote support teams aim to boost efficiency, reduce costs, and increase customer satisfaction.
Unity’s integrated approach streamlines and transforms contact center workflows while automating administrative tasks, incident triage, compliance, communication, and robust self-service, thus enabling significant operational efficiencies while dramatically lowering human level of effort.
AI is perfect—until it isn’t. We know end users have a tipping point. Our solutions include humans in the loop.
Stewarding the technology to deliver healthcare throughout hospitals, health systems, and physician groups



